Abstract
Research Article
Clinical characteristics in STEMI-like aortic dissection versus STEMI-like pulmonary embolism
Oscar MP Jolobe*
Published: 31 July, 2020 | Volume 4 - Issue 1 | Pages: 019-030
Dissecting aortic aneurysm with ST segment elevation, and pulmonary embolism with ST segment elevation are two of a number of clinical entities which can simulate ST segment elevation myocardial infarction.
Objective: The purpose of this review is to analyse clinical features in anecdotal reports of 138 dissecting aortic aneurysm patients with STEMI-like presentation, and 102 pulmonary embolism patients with STEMI-like presentation in order to generate insights which might help to optimise triage of patients with STEMI-like clinical presentation.
Methods: Reports were culled from a literature search covering the period January 2000 to March 2020 using Googlescholar, Pubmed, EMBASE and MEDLINE. Reports were included only if there was a specification of the location of ST segment elevation and an account of the clinical signs and symptoms. Search terms were “ST segment elevation”,”aortic dissection”, “pulmonary embolism”, “myocardial infarction”, and “paradoxical embolism”. Fisher’s exact test was utilised for two-sided comparison of proportions. Proportion was calculated for each group as the number of patients with that parameter relative to the total number of patients assessed for that parameter.
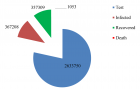
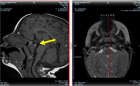
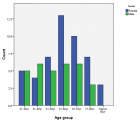
Findings: There were 138 patients with aortic dissection, 91 of whom were either fast-tracked to coronary angiography (81 patients) or fast-tracked to thrombolytic treatment (10 patients). There were 47 patients managed with neither of those strategies. There were 102 patients with pulmonary embolism, 71 of whom were fast tracked to coronary angiography, and 31 who did not receive that evaluation. Compared with their dissecting aortic aneurysm counterparts, those dissecting aortic aneurysm patients initially managed by percutaneous coronary intervention or by thrombolysis were significantly (p = 0.0003) more likely to have presented with chest pain, and significantly (p = 0.018) less likely to have presented with breathlessness. The preferential fast-tracking to coronary angiography prevailed in spite of comparable prevalence of back pain in fast tracked and in non-fast tracked subjects. Use of transthoracic echocardiography was also comparable in the two subgroups of dissecting aortic aneurysm patients. Pulmonary embolism patients fast tracked to percutaneous coronary intervention were significantly (p = 0.0008) more likely to have presented with chest pain than their pulmonary embolism counterparts who were not fast-tracked. The prevalence of paradoxical embolism was also significantly (p = 0.0016) higher in fast-tracked patients than in counterparts not fast-tracked. Cardiac arrest was significantly (p = 0.0177) less prevalent in fast-tracked pulmonary embolism patients than in pulmonary embolism patients who were not fast-tracked. Preferential fast-tracking to coronary angiography prevailed in spite of the fact that prevalence of documented deep vein thrombosis was comparable in fast-tracked subjects and in subjects not fast-tracked. The prevalence of use of transthoracic echocardiography was also similar in fast-tracked pulmonary embolism patients vs counterparts not fast tracked. Overall, however, transthoracic echocardiography had been utilised significantly (p = 0.007) less frequently in dissecting aneurysm patients than in pulmonary embolism patients.
Conclusion: Given the high prevalence of STEMI-like presentation in aortic dissection there is a need for greater use of point-of-care transthoracic echocardiography to mitigate risk of inappropriate percutaneous coronary intervention(which might delay implementation of aortic repair surgery) and inappropriate thrombolysis(which might precipitate hemorrhagic cardiac tamponade) (75) during triage of patients presenting with ST segment elevation simulating ST segment elevation myocardial infarction (STEMI). Furthermore, during triage of patients with STEMI-like clinical presentation, the combined use of point-of -care echocardiography and evaluation for deep vein thrombosis will facilitate the differentiation between acute myocardial infarction, STEMI-like aortic dissection, and STEMI-like pulmonary embolism. Among STEMI-like patients in whom DAA has been ruled out by point of care TTE, fast tracking to PCI might generate an opportunity to identify and treat paradoxical coronary artery embolism by thrombectomy. Thereby mitigating the mortality risk associated with coronary occlusion. Concurrent awareness of PE as the underlying cause of paradoxical embolism also generates an opportunity to relieve the clot burden in the pulmonary circulation, either by pulmonary embolectomy or by thrombolysis. Above all, frontline clinicians should have a greater awareness of the syndrome of STEMI-like presentation of aortic dissection and STEMI-like pulmonary embolism so as to mitigate the risk of inappropriate thrombolysis and inappropriate percutaneous coronary angiography which seems to prevail even in the presence of red flags such as back pain (for aortic dissection) and deep vein thrombosis(for pulmonary embolism).
Read Full Article HTML DOI: 10.29328/journal.avm.1001013 Cite this Article Read Full Article PDF
Keywords:
Aortic dissection; Pulmonary embolism; ST-elevation; Percutaneous coronary intervention
References
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012; 33: 2551-2567. PubMed: https://pubmed.ncbi.nlm.nih.gov/22922414/
- Wang JL, Chen CC, Wang CY, Hsieh MJ, Chang SH, et al. Acute Type A aortic dissection presenting as ST segment elevation myocardial infarction referred for percutaneous coronary intervention. Act Cardiol Sinica. 2016; 32: 265-272. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4884753/
- Villablanca PA, Vlismas PP, Aleksandrovich T, Omondi A, Gupta T, et al. Case report and systematic review of pulmonary embolism mimicking ST-elevation myocardial infarction. Vascular. 2019; 27: 90-97. PubMed: https://pubmed.ncbi.nlm.nih.gov/30056785/
- Fabris E, Arrigoni P, Falco L, Barlati G, Stolfo D, et al. Impact of patient delay in a modern real world STEMI network. Am J Emerg Med. 2020.
- Nazerian P, Mueller C, de Matos Soeiro, Leidel BA, Salvadeo SAT, et al. Diagnostic accuracy of the aortic dissection risk score plus D-dimer for acute aortic syndromes. Circulation. 2018; 137: 250-258. PubMed: https://pubmed.ncbi.nlm.nih.gov/29030346/
- Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: Increasing the model’s utility with the simpliRED D-dimer. Thromb Haemost 2000; 83: 416-420. PubMed: https://pubmed.ncbi.nlm.nih.gov/10744147/
- Hibi K, Kimura K, Nakatogawa T, Okuda J, Umcumura S, et al. Intracoronary ultrasound diagnosis of an aortic dissection causing anterior acute myocardial infarction. Circulation. 2003; 108: e145-e146.
- Wang ZG, Zhao W, Shen BT, Zheng Y, Liu Q. Successful treatment of a case of acute myocardial infarction due to type A aortic dissection by coronary artery stenting: A case report. Exper Therap Med. 2015; 10: 759-762. PubMed: https://pubmed.ncbi.nlm.nih.gov/26622389/
- Wang W, Wu J, Zhao XZ, You K, Li C. Type A aortic dissection manifesting as acute inferior myocardial infarction: 2 case reports. Medicine. 2019; 98: 43: e17662. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6824788/
- Wang JY, Su X, Li CW, Zhang ZP, Song D, et al. Acute myocardial infarction could induce aortic dissection. Int J Cardiovasc Dis Diag. 2017; 2: 001-003.
- Wang D, Zhang LL, Wang ZY, Wang Y. The missed diagnosis of aortic dissection in patients with myocardial infarction: a disastrous event. J Thoracic Dis. 2017; 9: E636-E639. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5542992/
- Chen A, Ren X. Aortic dissection manifesting as ST-segment-elevation myocardial infarction. Circulation. 2015; 131: e503-e504.
- Yunoki K, Naruko T, Itoh A, Furakawa A, Abe Y, et al. Stenting of right coronary ostial occlusion due to thrombosed type A aortic dissection: One year follow-up results. J Cardiol Cases. 2010; 1: e166-e170. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6264950/
- Doksoz A, Ozturk MT, Salha W, Taraktas M, Soydemir H. A case of aortic dissection complicating right subclavian artery occlusion and mimicking myocardial infarction. Emerg Case Rep. 2011; 8: 40-42.
- Cardozo C, Riadh R, Mazen M. Acute myocardial infarction due to left main stem compression aortic dissection treated by direct stenting. JIC. 2004: 16.
- Baydar O, Abaci O, Cetinkal G, Oktay V, Kocas C, et al. PP-227 Acute myocardial infarction due to acute aortic dissection involving the left main coronary artery. Int J Cardiol. 2013; 163: Suppl 1: S171.
- Rodrigues RC, Santos N, Pereira D. Aortic dissection mimicking ST elevation myocardial infarction. Acta Med Port. 2017; 30: 80-80.
- Tsigkas G, Kasimis G, Theodoropoulos K, Chouchoulis K, Balkoussis NG, et al. A successfully thrombolysed acute inferior myocardial infarction due to Type A aortic dissection with lethal consequences; the importance of early cardiac echocardiography. J Cardiothoracic Surg. 2011; 6: 101. PubMed: https://pubmed.ncbi.nlm.nih.gov/21864356/
- Sir JJ, Kim YI, Cho WH, Choi SK. Acute myocardial infarction due to aortic dissection. Intern Med. 2009; 48: 173. PubMed: https://pubmed.ncbi.nlm.nih.gov/19182429/
- Okamoto M, Amano T, Matsuoka S, Hirai H, Masuda K, et al. A case of acute myocardial infarction due to left main trunk occlusion complicated with acute dissection as diagnosed by intravascular ultrasound. Cardiol Res. 2012; 3: 232-235. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5358137/
- Kawano H, Tomichi Y, Fukae S, Koide Y, Tode G, et al. Aortic dissection associated with acute myocardial infarction and stroke found at autopsy. Internal Med. 45: 957-962. PubMed: https://pubmed.ncbi.nlm.nih.gov/16974058/
- Gu YL, van den Heuvel AFM, Erasmus ME, Ziljstra F. Aortic dissection presenting as acute myocardial infarction potential harm of antithrombin and antiplatelet therapy. Netherlands Heart J. 2006; 14: 147-149. PubMed: https://pubmed.ncbi.nlm.nih.gov/25696613/
- Dendramis G, Fazzari F, Paleologo C, Asciutto S. Acute aortic dissection debut as STEMI; A case report. J Indian Coll Cardiol. 2014; 4: 182-185.
- Kwon YS, Lee HS, Shin KJ, Chang BJ, Kim HS, et al. A case of left main coronary stenting for acute myocardial infarction complicated by ascending aortic dissection. Korean Circulat J. 2004; 34: 1210-1215.
- Masuda Z, Murakami T, Shishido E, Kuinose M. A rare cause of dissection of ascending aorta after aortic valve replacement. Asian Cardiovasc Thorac Ann 2008; 16: 4-6.
- Almansoni M, Tymchak W. Aortic dissection and sudden unexpected deaths: A retrospective study of 31 forensic autopsy cases. J Forensic Sci. 2015.
- Siddiqui S, Kwan CNK, Concepcion J, Malik BA, Moskovitz N, et al. A unique case of acute dissection mimicking myocardial infarction. J Case Rep Images Med. 2017; 3: 53-57.
- Ahmed T, Nair R, Lak H, Lodhi SH, Maroo A. Two intriguing cases of Stanford Type A acute aortic dissection. Cureus 2020; 12: e6986. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075513/
- Irivbogbe O, Mirrer B, Loarte P, Gale M, Cohen R. Thrombolytic-related complication in a case of misdiagnosed myocardial infarction. Acute Cardiac Care. 2014; 16: 83-87. PubMed: https://pubmed.ncbi.nlm.nih.gov/24749992/
- Guner EG, Agus H, Guner A, Kalkan AK, Ertuk M. Spontaneous aortic root rupture during pregnancy. Turk Kardiyol Dern Ars. 2020; 48: 186.
- Gibbs O, Faour A, Femia G, Nguyen T, Lo S. Inferior ST elevation myocardial infarction secondary to type A aortic dissection treated with percutaneous coronary intervention immediately prior to urgent ascending aortic repair. Heart Lung Circulat. 2018; 27: S456-S457.
- Danbauchi SS, Ibinaiye PO, Anyiam CA, Ahlassan MA, Oyati AI. DeBakey type 1 aortic dissection presenting as inferior myocardial infarction: A case report and review of literature. Arc Int Surg. 2013; 3: 154-157.
- Zschaler S, Schmidt G, Kukucka M, Syrmas G, Zaschke L, et al. How to prevent inadvertent emergency anticoagulation in acute type A aortic dissection: when in doubt, don’t. Cardiovasc Diagn Ther. 2018; 8: 805-810. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331368/
- Massetti M, Neri E, Babatesi G, Le Page O, Sabatier R, et al. Flap suffocation: An uncommon mechanism of coronary malperfusion in acute type A dissection. J Thoracic Cardiovascular Surg. 2003; 125: 1548-1550.
- Zakaria S, Desai D, Jeudy J, Thorn EM. Aortic dissection and pericardial tamponade causing compression of the pulmonary arteries in a patient with prior cardiac surgery. J Card Surg. 2011; 26: 316-321.
- He X, Liu X, Li W, Gao B, Zeng H. Acute Stanford type A aortic dissection occurred simultaneously with acute myocardial infarction. Int J Cardiol. 2013; 189: 56-58.
- Laine M, Grisoli D, Bonello L. An atypical case of acute myocardial infarction. JIC. 2011; 23: 305-306.
- Omar AR, Goh WP, Lim YT. Peripartum acute anterior ST segment elevation myocardial infarction: An uncommon presentation of acute aortic dissection. Ann Acad Med Singapore. 2007; 36: 854-856. PubMed: https://pubmed.ncbi.nlm.nih.gov/17987238/
- Fossum E, Ata B, Eritsland J, Klow NE, Mangschau A. Thoracic aortic dissection-an important differential diagnosis of chest pain and ECG changes. Tidsskriftet Den Norse Legeforening. J Norwegian Med Assoc. 2003; 123: 2431-2432.
- Tang L, Hu XQ, Zhou SH. Acute Stanford type A aortic dissection mimicking acute myocardial infarction: A hidden catastrophe which should prompt greater vigilance. Acta Cardiol Sin. 2014; 30: 493-496. PubMed: https://pubmed.ncbi.nlm.nih.gov/27122825/
- Cook J, Aeschlimann S, Fuh A, Kohmoto T, Chang SM. Aortic dissection presenting as concomitant and STEMI. J Human Hypertens. 2007; 21: 818-821.
- Sung LC, Kuo CH, Hou CJY, Tsai CH. Acute myocardial infarction caused by ascending aortic dissection. Acta Cardiol Sin. 2005; 21: 105-110.
- Fujiyoshi T, Koizumi N, Nishibe T, Sugiyama K, Ogino H. Direct repair of localized aortic dissection with critical malperfusion of the left main trunk. Ann Thorac Cardiovasc Surg. 2018; 24: 320-323. PubMed: https://pubmed.ncbi.nlm.nih.gov/29386473/
- Courand PY, Dauohin R, Roussel E, Besnard C, Lanteime P. An uncommon presentation of acute Type A aortic dissection: left main coronary artery obstruction. Images Cardiovasc Med. 2012; 13: 53-55.
- Hirata K, Wake M, Kyushima M, Takahashi T, Nakazato J, et al. Electrocardiographic changes in patients with type A aortic dissection. Incidence, patterns and underlying mechanisms in 159 cases. J Cardiol. 2010; 56: 147-153. PubMed: https://pubmed.ncbi.nlm.nih.gov/20434885/
- Radwan K, Peszek-Przybyia E, Gruszka A, Sonsowski M, Buszman P. Acute aortic dissection imitating ST elevation myocardial infarction with accompanying pulmonary embolism. Cardiol J. 2007; 14: 595-596.
- Ruisi M, Fallahi A, Lala M, Kanei Y. Aortic dissection presenting as acute subtotal left main coronary artery occlusion: A case approach and review of the literature. J Clin Res. 2015; 7: 356-360. PubMed: https://pubmed.ncbi.nlm.nih.gov/25780485/
- Kozinski L, Orzalkiewicz M, Lica-Gorzyynska M, Orzalkiewicz Z. Left main stem pulsation:easily missed angiographic phenomenon in acute aortic dissection. European Heart J. 2015; 36: 129. PubMed: https://pubmed.ncbi.nlm.nih.gov/25157111/
- Na SH, Youn TJ, Cho YS, Lim C, Chung WY, et al. Acute myocardial infarction caused by extension of a proximal aortic dissection flap into the right coronary artery. Circulation. 2006; 113: e669-e671.
- Ravandi A, Penny WF. Percutaneous intervention of an acute left main coronary occlusion due to dissection of the aortic root. JACC Cardiovasc Interven. 2011; 4: 713-715.
- Lentini S, Specchia L, Cricco A, Mangia F, Ignone G, et al. Hybrid management of acute type A aortic dissection presenting as acute coronary syndrome. Int J Cardiol. 2013; 167: e85-e87. PubMed: https://pubmed.ncbi.nlm.nih.gov/23664702
- Treptau J, Ebnet J, Akin M, Tongers J, Bauersachs J, et al. Angiographic detection of fatal acute aortic dissection Stanford Type A under resuscitation. Cardiol J. 2016; 23: 620-622. PubMed: https://pubmed.ncbi.nlm.nih.gov/27976792/
- Attia T, Robichi M, Lincoff AM, Shishehbor MH, Svenson L, et al. Successful treatment of aortic root dissection complicated with extensive myocardial infarction using the total artificial heart. J Case Rep. 2017; 8: 1-3.
- Barabas M, Gosselin G, Crepeau J, Petitclerc R, Cartier R, et al. Left main stenting as a bridge to surgery for acute type A aortic dissection and anterior myocardial infarction. Catheterisation and Cardiovascular Interventions 2000; 51: 74-77.
- Wu BT, Li CY, Chen YT. Type A aortic dissection presenting with inferior DT-elevation myocardial infarction. Acta Cardiol Sin. 2014; 30: 248-252. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804865/
- Hawatmeh A, Arqoub AA, Isbitan A, Shamoon F. A case of ascending aortic dissection mimicking acute myocardial infarction and complicated with pericardial tamponade. Cardiovasc Diagn Ther. 2016; 6: 166-171. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4805766/
- Erkan H, Cirakoglu OF, Erkan M. Aortic dissection flap imitating thrombus: an extremely rare angiographic presentation of myocardial infarction. J Intervent Cardiol. 2105; 28: 117-118.
- Pinney SP, Wasserman HS. Anterior myocardial infarction, acute aortic dissection, and anomalous coronary artery. J Interven Cardiol. 2002; 15: 293-296. PubMed: https://pubmed.ncbi.nlm.nih.gov/12238425/
- Horszczaruk G, Roik MF, Kochman J, Bakon L, Stolarz P, et al. Aortic dissection involving ostium of right coronary artery as the reason for myocardial infarction. Eur Heart J. 2006; 27: 518. PubMed: https://pubmed.ncbi.nlm.nih.gov/16243924/
- Zegers ES, Gehlmann HR, Verheuger FWA. Acute myocardial infarction due to an acute type A aortic dissection involving the left main coronary artery. Neth Heart J. 2007; 15: 263-264. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1995115/
- Lee CH, Lim J. Type A aortic dissection: a hidden and lethal cause for failed thrombolytic treatment in acute myocardial infarction. Heart. 2007; 93: 825. PubMed: https://pubmed.ncbi.nlm.nih.gov/17569805/
- Chammarnphol N, Cheewatanakornkul S, Wisaratapong T. Coronary spasm due to type A aortic dissection complicated by hemopericardium: case report of another possible cause of coronary malperfusion. Intern Med. 2010; 49: 829-831.
- Lee MJ, Park YS, Ahn S, Sohn CH, Seo DW, et al. Clinical features of acute aortic dissection patients initially diagnosed with ST segment elevation myocardial infarction. Cardiovasc. 2016; 27: 30-35.
- Phowthongkum P. Acute aortic dissection mimics acute inferoposterior wall myocardial infarction in a Marfan syndrome patient. BMJ Case Rep. 2010. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028170/
- Arrivi A, Tanzilli G, Puddu PE, Truscelli G, Dominici M, et al. Acute aortic dissection mimicking STEMI in the catheterization laboratory: Early recognition is mandatory. Case Rep Cardiol. 2012: 367542. PubMed: https://pubmed.ncbi.nlm.nih.gov/24826248
- Arrivi A, Tanzilli G, Tritapepe L, Mazzesi G, Mangieri E. Undetected acute aortic dissection in a patient referred for primary coronary angioplasty: a successful treatment of perioperative bleeding after abciximab administration. BMJ Case Rep. 2010. PubMed: https://pubmed.ncbi.nlm.nih.gov/22802278/
- Ali RG, Chrissoheris MP. Lead aVR ST segment elevation in acute aortic dissection. Connecticut Medicine 2008; 72: 19-20.
- Hsu PC, Su HM, Lin TS, Huang JW, Lai WT, et al. Acute type A aortic dissection involving right coronary artery orifice in a case presenting with anterior ST elevation. A Rare Case Rep Cardiol. 2011; 119: 11-14.
- Kaya MG, Mavill E, Dogdu O, Dogan A, Inanc T, et al. Acute type A aortic dissection in a patient with ventricular septal defect. Cardiovasc Revascularization Med. 2010; 11: 186-188.
- Inoue T, Fukumoto Y, Mohri M, Inokuchi K, Hirakawa Y, et al. Wandering ST segment elevation. Circulation. 2003; 108: e102-e103.
- Huang CY, Hung YP, Lin TH, Chang SL, Lee WL, et al. Catheter directed diagnosis of ST-segment elevation myocardial infarction induced by type A aortic dissection. Medicine. 2020; 99: e18796. PubMed: https://pubmed.ncbi.nlm.nih.gov/32011481/
- Sadaba M, Subinas A, Rumoroso JR. STEMI with fluctuating closing of LAD and Cx. Do not concentrate on the finger. Cardiovasc Revascularization Med. 2017; 18: S35-S39.
- Hanaki Y, Yumoto K, Seigen I, Aoki H, Fukuzawa T, et al. Coronary stenting with cardiogenic shock due to acute ascending aortic dissection. World J Cardiol. 2015; 26: 104-110. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4325300/
- Szabo S, Hoffmeister HM. Aortic dissection causing 2 myocardial infarctions. J Cardiol Cardiovasc Med. 2019; 4: 233-235.
- Harlandt O, Kupper W, Rebolledo Godoy M, Frenkel C, Lankisch PG. Fatal outcome of prehospital thrombolysis in a case of aortic dissection mimicking ST segment elevation myocardial infarction. Intensivmedizin und Notfallmedizin 2006; 43: 219-225.
- Latifi AN, Ibe U. ST-elevation myocardial infarction: rare presentation of an uncommon disease. CHEST. 2019; 156 (4 Suppl): A1471.
- Ali OM, White B. Trapdoor ischemia coronary ostial occlusion by an aortic dissection. BMJ Case Rep 2012.
- Lee MJ, Park YS, Ahn S, Sohn CH, Seo DW, et al. Clinical features of acute aortic dissection patients initially diagnosis with ST-segment elevation myocardial infarction. Cardiovascular. 2016; 27: 30-35.
- Ichihashi T, Ito T, Murai S, Ikehara N, Fujita H, et al. Acute myocardial infarction due to spontaneous localized acute dissection of the sinus of Valsalva detected by intravascular ultrasound and electrocardiogram-gated computed tomography. Heart Vessels. 2016; 31: 1570-1573. PubMed: https://pubmed.ncbi.nlm.nih.gov/26710761/
- Nandan AY, Singh A, Negesh NM, Gandhi M. Suspected ST segment elevation myocardial infarction referred for primary angioplasty: a masquerader. BMJ Case Rep. 2019; 12: e227687.
- Kaul P. Spontaneous retrograde dissection of ascending aorta from descending thoracic aorta-a case review. Perfusion. 2011; 26: 215-222.
- Palmeira MM, Ribeiro HYU, Lira YC, Neto FOM, da Silva Rodrigues IA, et al. Aortic aneurysm with complete atrioventricular block and acute coronary syndrome. BMC Research Notes. 2016; 9: 257. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4855812/
- Camaro C, Wouters NTAE, Gin MTJ, Bosker HAB. Acute myocardial infarction with cardiogenic shock in a patient with acute aortic dissection. Am J Emerg Med. 2009; 27: 899 -899.
- Cai J, Cao Y, Yuan H, Yang K, Vhu YS. Inferior myocardial infarction secondary to aortic dissection associated with bicuspid aortic valve. JCDR. 2012; 3: 138-142. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354459/
- Stefanidis C, Sanoussi A, Demanet H, Castro-Rodriguez, Wauthy P. Acute myocardial infarction due to an acute aortic dissection. Rev Med Brux. 2011; 32: 179-181.
- Scott C, Burruss N, Kalimi R, Manetta F, Palazzo RS, et al. Acute ascending aortic dissection during pregnancy. Am J Criticalare. 2001; 10: 430.
- Marek D, Nemec P, Herman M, Gwozdziewicz M, Troubil M, et al. Mistakes in dealing with aortic dissection, lessons from three warning cases. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2008; 152: 283-287.
- Jaguszewski M, Widmer N, Ghadri JR, Alibegovic J, Gaemperli O, et al. Haemodynamic tracing pattern revels acute type A aortic dissection. Acute Cardiac Care. 2012; 14: 94-95.
- Kubiak G, Gianowska G, Kubiak L, Traczewska M, Nowalany-Kozielska E. Acute aortic syndrome mimicking anterior wall ST-elevation myocardial infarction. Kardiologia Polska. 2013; 71: 852-854.
- Boulaamayl El Fatemi S. Acute aortic syndrome mimicking myocardial infarction. Eur Heart J Cardiovasc Imaging. 2015 (Suppl 1): 127.
- Guo XM, Bonde P. Ruptured pneumococcal aortic aneurysm presenting as ST-elevation myocardial infarction. AORTA. 2015; 3: 30-37. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714936/
- Chenkin J. Diagnosis of aortic dissection presenting as ST-elevation myocardial infarction using point-of –care ultrasound. J Emerg Med. 2017; 53: 880-884. PubMed: Chttps://pubmed.ncbi.nlm.nih.gov/29066079/
- Abrams E, Allen A, Lahham S. Aortic dissection with subsequent hemorrhagic tamponade diagnosed with point-of –care ultrasound in a patient presenting with STEMI. Clin Pract Cases Emerg Med. 2019; 3; 103-106. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6497200/
- Wang Y, Zhu Z, Xu R, Li D, Wang T, et al. A complete occlusion of right coronary artery due to Stanford Type A aortic dissection. Successful treatment with extracorporeal membrane oxygenation. Bra J Cardiovasc Surg. 2019; 34: 491-494. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6713360/
- Pocar M, Passolunghi D, Moneta A, Donatelli F. Recovery of severe neurological dysfunction after restoration of cerebral blood flow in acute aortic dissection. Interac Cardiovasc Thoracic Surg. 2010; 10: 839-842.
- Ohtani N, Kiyokawa K, Asada H, Kawakami T. Stanford type A acute dissection developing acute myocardial infarction. JJTCVS. 2000; 48: 69-72.
- Ashida K, Arakawa K, Yanagishi T, Tahara T, Ayaori M, et al. A case of aortic dissection with transient ST segment elevation due to functional left main coronary artery obstruction. Jpn Circ J. 2000; 64: 130-134. PubMed: https://pubmed.ncbi.nlm.nih.gov/10716527/
- McBeth BD, Rosenstein DI. Acute aortic dissection with ST segment myocardial infarction following masturbation. J Emerg Med. 2020; 58: E193-E196. PubMed: https://pubmed.ncbi.nlm.nih.gov/32204992/
- Fernandez-Jimenez R, Vivas D, de Augustin JA, Kallmeyer A, Balbacid E,
et al. Acute aortic dissection with ongoing right coronary artery and aortic valve involvement. Int J Cardiol. 2012; 161: e34-e36 - Sherwood JT, Gill IS. Missed acute ascending aortic dissection. J Card Surg. 2001; 16: 86-88.
- Kamata S, Funatsu T, Itou Y, Yagihara T. Conservatively treated coronary malperfusion associated with acute type A dissection before aortic root replacement. J Cardiol Cases. 2018; 17: 36-39. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6149557/
- Al-Wahibi K, Al-Dhuhli H, Diputado T, Alzadjali N. Acute cardiovascular emergency; missed killer in the emergency room. Oman Med J. 2008; 23: 112-115. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3282426/
- Ohuchi H, Kyo S, Matsumura M, Tanabe H, Asano H, et al. Global myocardial ischaemia as a complication of Type A aortic dissection. Jpn Circ J. 2000; 64: 533-536.
- Li SW, Osman M. Thoracic aortic aneurysm (TAA)-A diagnostic dilemna in a patient with hemoptysis. M0JEM 2017; 2: 23-27.
- Beggs A, Al-Rawi H, Parfitt A. Chest pain and fleeting neurological signs. Lancet. 2005; 365: 1514.
- Thota LTD, Zanoni LTS, Mells C, Auten JD. Acute proximal aortic dissection with negative D-dimer assay and normal portable chest radiograph: A Case Report. Military Med. 2015; 180: e164-e167.
- Correale M, Di Martino L, Ieva R, Di Biase M, Brunetti ND. Aortic dissection after cocaine abuse. Clin Res Cardiol. 2011; 100: 1129-1130.
- Ascione L, Accadia M, damiano S, De Michele M, Tuccillo B. Painless acute aortic dissection presenting as echocardiographically diagnosed left ventricular outflow obstruction. Ital Heart J. 2002; 3: 752-754. PubMed: https://pubmed.ncbi.nlm.nih.gov/12611129/
- Ngermsritrakul T, Sathirapanya P. Type A aortic dissection presenting as acute ischemic stroke. Caution for thrombolytic therapy; a case report and literature review. J Med Assoc Thai. 2008; 91: 1302-1307.
- Theodosis-Georgilas A, Beidekos D. Aortic dissection involving the ostium of left main coronary artery. Hospital Chronicles 2009; 4: 91-94.
- Abdelnaby M, Abada M, Elsayed A, Dawood M, Saleh Y, et al. Painless aortic dissection presented with acute paraplegia. Int J Cardiovasc Acad. 2019; 5: 22-24.
- D’Aloia A, Vizzardi E, Bugatti S, Magatelli M, Bonadei I, et al. A Type A aortic dissection mimicking an acute myocardial infarction. Cardiol Res. 2012; 3: 94-96. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5358147/
- Gudivada KK, Umesh K, Sudeendrababu ARB. Complete heart block in acute aortic dissection: An unusual presentation. Am J Med Sci. 2018; 356: e39-e40.
- Alsaad AA, Odunukan OW, Patton JN. Ascending aortic dissection presented as inferior myocardial infarction: a clinical and diagnostic mimicry. BMJ Case Rep. 2016.
- Kodera S, Ikeda M, Sato K, Kushida S, Kanda J. Percutaneous coronary intervention is a useful bridge treatment for acute myocardial infarction due to acute type A aortic dissection. Cardiovasc Interv and Ther. 2015; 30: 61-67.
- Li CH, Leta R, Pons-Llado G. Myocardial hypoperfusion in acute aortic dissection. Rev Esp Cardiol. 2014; 67: 323. PubMed: https://pubmed.ncbi.nlm.nih.gov/24774597/
- Guvenc TS, Erer HB, Cetin R, Hasdemir H, Iihan E, et al. Acute aortic regurgitation with myocardial infarction: an important clue for aortic dissection. J Emerg Med. 2013; 44: e5-e8. PubMed: https://pubmed.ncbi.nlm.nih.gov/22305147
- Tarver K, Kindler H, Lythall D. Extensive aortic dissection presenting as acute inferior myocardial infarction. Heart. 2007; 93: PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2000954/
- Katayama A, Uchida N, Sutoh M, Sueda T. Partial remodelling on the two sinuses for acute type A aortic dissection with right coronary arterial dissection. Ann Vasc Dis. 2013; 6: 666-669.
- Amabile N, Foin N, Girard MJ, Dabauchez M, Caussin C. Left main artery compression by haematoma following acute aortic root dissection: identification by optical coherence tomography. European Heart J Cardiovasc Imaging. 2016; 17: 1317. PubMed: https://pubmed.ncbi.nlm.nih.gov/27458184/
- Tomaszuk-Kazberuk A, Sobkowicz B, Lewezuk A, Prokop A, Sawicki R, et al. Silent pulmonary embolism in a patient with myocardial infarction and type B acute aortic dissection-a case report. Adv Med Sci. 2010; 55: 99-102.
- Ayrik C, Cece H, Aslon O, Karcioglu O, Yilmaz E. Seeing the invisible: painless aortic dissection in the emergency setting. Emerg Med J. 2006; 23:e24. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2464426/
- Monteiro P, Vieira A, Parreira M. Aortic aneurysm dissection-diagnosis may be hard to make. Medicina Interna. 2009; 16; 211-215.
- Gomez-Polo JC, Aguilar-Navarro E, Olmos C, Rosillo S, Garcia-Diego G, et al. Atrial Septum Hematoma - Another Way to Die in Acute Aortic Dissection. Circ J. 2017; 81: 1370-1372. PubMed: https://pubmed.ncbi.nlm.nih.gov/28344204/
- Panneerselvam A, Dattatreya PV, Sridhar L, Prabhavathi B, Nanjappa M. ST-segment elevation in right precordial leads in acute pulmonary embolism. J Indian Coll Cardiol. 2011; 1: 112-114.
- Zhang F, Qian J, Dong L, Ge J. Multiple ST-segment elevations in anterior and inferior leads: An unusual electrocardiographic manifestation in acute pulmonary embolism. Int J Cardiol. 2012; 160: e18-e20.
- Emren SV, Arikan ME, Senoz O, Varis E, Akan E. Acute pulmonary embolism mimicking inferior myocardial infarction. Arch Turk Soc Cardiol. 2014; 42: 290-293. PubMed: https://pubmed.ncbi.nlm.nih.gov/24769824/
- Sadeghpour A, Alizadeasl. Can isolated ST elevation in aVR lead be a sign of acute pulmonary embolism. Anadolu Kardiyol Derg. 2013; 13: 286-294.
- Zelfani S, Manal H, Laabidi S, Wahabi A, Akeri S, et al. Pulmonary embolism mimicking acute myocardial infarction: a case report and review of the literature. Pan African Med J. 2019; 33: 275. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6814957/
- Bozorgi A, Rahnamoun Z. Pulmonary thromboembolism initially mistaken for inferior STEMI. Herz. 2013; 38: 553-555.
- Beygui F, Tran H, Montalescot G. Chest pain, ST segment elevation in aVR lead, and high troponin levels. Arc Cardiovasc Dis. 2009; 102: 79-80. PubMed: https://pubmed.ncbi.nlm.nih.gov/19233114/
- Raghav KPS, Makkuni P, Figueredo VM. A review of electrocardiography in pulmonary embolism: Recognizing pulmonary embolus masquerading as ST elevation myocardial infarction. Rev Cardiovasc Med. 2011; 12: 157-163. PubMed: https://pubmed.ncbi.nlm.nih.gov/22145193/
- Budavari AI, Glenn TJ, Will KK, Askew JW, Fortuin FD. A case of simultaneous pulmonary embolism and acute myocardial infarction secondary to a previously undiagnosed patent foramen ovale. J Hosp Med. 2009; 4: E5-E8. PubMed: https://pubmed.ncbi.nlm.nih.gov/19504585
- Wasek WC, Samul W, Ryczek R, Skrobowski A. Unique case of ST-Segment-elevation myocardial infarction related to paradoxical embolization and simultaneous pulmonary embolization. Circulation. 2015; 131: 1214-1223.
- Yildiz A, Bostan C, Akin F, Ozkan AA, Gurmen T. Concurrent pulmonary embolism and acute coronary syndrome with dynamic electrocardiographic changes. Am J Emerg Med. 2012; 30: 637.e1-4. PubMed: https://pubmed.ncbi.nlm.nih.gov/21450430/
- Goslar T, Podbregar M. Acute ECG ST-segment elevation mimicking myocardial infarction in a patient with pulmonary embolism. Cardiovasc Ultrasound. 2010; 8; 50. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3002912/
- Gul EE, Nikus KC, Erdogan H, Ozdemir K. Differential diagnostic dilemna between pulmonary embolism and acute coronary syndrome. J Arrhythmia. 2016; 32: 160-161. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4823566/
- Ozer N, Yorgun H, Canpolat U, Ates AH. Pulmonary embolism presenting with evolving electrocardiographic abnormalities mimicking anteroseptal myocardial infarction: a case report. Med Princ Pract. 2011; 20: 577-580. PubMed: https://pubmed.ncbi.nlm.nih.gov/21986020/
- Fallahi MJ, Masoompour M, Mirzaee M. Pulmonary embolism with abdominal pain and ST elevation: A Case Report. Iran J Med Sci. 2014; 39: 395-398. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4100053/
- Piywaczewska M, Piotrowska-Kownacka D, Zdonczyk O, Roik M, Jankowski K, et al. Two in one: Unexpected acute pulmonary embolism detected by cardiovascular magnetic resonance in a patient with acute myocarditis. Cardiol J. 2017; 24: 96-97. PubMed: https://pubmed.ncbi.nlm.nih.gov/28245048/
- Abdalla A, Kelly F. STEMI-like acute pulmonary embolism, an unusual presentation. BMJ Case Rep. 2014; 2014: bcr2014206517. PubMed: https://pubmed.ncbi.nlm.nih.gov/25414218/
- Akgedik R, Gunayadin ZY, Yildirim BB, Dagli CE, Bektas O. What should be done in the event of simultaneous pulmonary embolism and myocardial infarction with ST elevation? Turk Kardiyol Dern Ars. 2015; 43: 734-738.
- Noble J, Singh AS. Asymptomatic pulmonary embolus masquerading as acute anteroseptal myocardial infarction. Can J Emerg Med. 2011; 13: 62-65.
- Navas MH, Barreda AP, Selman-Housein KH, Obregon-Santos AG, de Zayas Gaiguera YQB. Tromboembolismo pulmonary o infarto de ventriculo derecho: Dilema clinic, a proposito de un caso. CorSalud. 2015; 7: 243-247.
- Motazedian P, Le May MR, Glover C, Hibbert B. A woman on her 80s with anterior ST elevation myocardial infarction and shock. CHEST. 2017; 151: e5-e8.PubMed: https://pubmed.ncbi.nlm.nih.gov/28065257/
- Fasullo S, Paterna S, Di Pasquale P. An unusual presentation of massive pulmonary embolism mimicking septal acute myocardial infarction treated with tenecteplase. J Thrombosis Thrombolysis. 2009; 27: 215-219. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4350959/
- Livatidis IG, Paraschos M, Dimopoulos K. Massive pulmonary embolism with ST elevation in leads V1-V3 and successful thrombolysis with tenecteplase. Heart. 2004; 90: e41.PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768302/
- Montenegro FS, Barzan V, De Lorenzo AR, Pittella FJM, da Rocha ASC. ST-segment elevation in pulmonary thromboembolism. Arq Bras Cardiol. 2012; 99: e131-e133.
- Wilson GT, Schaller FA. Pulmonary embolism mimicking anteroseptal acute myocardial infarction. J Am Osteopath Assoc. 2008; 108: 344-349. PubMed: https://pubmed.ncbi.nlm.nih.gov/18648028/
- Roongsangmanoon W, Wongsoasup A, Rattanajaruskul N, Angkananard T. Acute pulmonary embolism masquerading as antroseptal myocardial infarction. J Med Assoc Thai. 2017; 100 Suppl 8: S221-S225.
- Alsidawi S, Abdalla M, Helmy T. Massive pulmonary embolism with ST elevation in the inferior leads and other interesting ECG findings. J Biomed Graph Computing. 2013; 3: 43-50.
- Grant-Orser A, Ballantyne B, Haddara W. Unique ECG findings in acute pulmonary embolism STE with reciprocal changes and pathologic Q wave. Case Rep CritCare. 2018; 2018: 7865894. PubMed: https://pubmed.ncbi.nlm.nih.gov/29850272/
- Toprak C, Avci A, Ozturkeri B, Tabakci MM, Kahveci G. PE with ST-segment elevation in leads V1-3 and AVR treated successfully by catheter directed high dose bolus thrombolytic therapy during CPR. Am J Emerg Med. 2014; 32: 1557 -1557.
- Oguzhan A. Percutaneous rotational pulmonary thrombectomy. N Engl J Med. 2016.
- Zhan ZQ, Wang CQ, Baranchuk A. Acute pulmonary embolism with ST segment elevation in the inferior leads. Int J Cardiol. 2014; 177: 718-719.
- Barsoum EA, Bhat T, McCord DA, Lafferty J. Uncommon presentation of fatal pulmonary embolism. Angiology. 2013; 1: 1-2.
- Mohammed K, Sasieta-Tello H, Badireddi S. Massive pulmonary embolism with ST elevation in leads V1-V3 and successful aspiration thrombectomy Case report and review of EKG changes in acute pulmonary embolism. J Med Cases. 2013: 4: 662-666.
- Agdamag A, Krishnappa D, Benditt DG. ST-segment changes after loss of consciousness. Circulation. 2020; 141: 80-82.
- Kameczura T, Rajzer M, Jankowski P, Wilinski J, Czarnecka D. Acute pulmonary embolism mimicking STEMI. Do the potential benefits of pulmonary artery angiography support the decision to perform the procedure? Przegl Lek. 2014; 71: 407-409.
- Lu YW, Tsai YL, Chang CC, Huang PH. A potential diagnostic pitfall in acute chest pain: massive pulmonary embolism mimicking acute STEMI. Amer J Emerg Med. 2018; 36: 461-463. PubMed: https://pubmed.ncbi.nlm.nih.gov/29169886/
- Shy BD, Gutierrez A, Strayer RJ. Bedside ultrasound to evaluate pulmonary embolism masquerading as ST elevation myocardial infarction (STEMI). J Emerg Med. 2015; 49: 703-704.
- Omar HR. ST segment elevation in V1-V4 in acute pulmonary embolism: a case presentation and review of the literature. European Heart J Acute Cardiovasc Care. 2016; 5: 579-586. PubMed: https://pubmed.ncbi.nlm.nih.gov/26373811/
- Kahyaoglu M, Alizade E, Naser A, Izgi A. Pulmonary embolism presenting with ST segment elevation in inferior leads. Int J Cardiovasc Academy. 2017; 3: 41-44.
- Yeh KH, Chang HC. Massive pulmonary embolism with anterolateral ST-segment elevation electrocardiogram limitations and the role of the echocardiogram. Amer J Emerg Med. 2008; 26: 632 -632.
- Nakata A, Aburadani I, Kontani K, Hirota S. Acute pericarditis following acute pulmonary thromboembolism. Int Heart J. 2017; 58: 1028-1033. PubMed: https://pubmed.ncbi.nlm.nih.gov/29151495/
- Lee DZJ, Whittaker M, Al-Mohammed A. An unusual presentation of pulmonary embolism. BMJ Case Rep. 2012; 2012:bcr2012006210. PubMed: https://pubmed.ncbi.nlm.nih.gov/22878987/
- Yamagami F, Mizumo A, Shirai T, Niwa K. A savage sequence: ST elevations with pulmonary embolism. Am J Med. 2014.
- Velasco CE, Howard C. Trouble on both sides: Pulmonary embolism with pneumothorax. Amer J Med. 2017; 130: 530-533. PubMed: https://pubmed.ncbi.nlm.nih.gov/28159603/
- Manne JRR. Acute ST segment elevation in a patient with massive pulmonary embolism mimicking acute left main coronary obstruction. JACC. 2017.
- Pavlidis AN, Poulimenos LE, Giannakopoulos AK, Tsoukas A, Kallistratos MS, et al. Electrocardiographic changes in a patient with pulmonary embolism and septic shock. Korean Circ J. 2011; 41: 692–693. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3242029/
- Sheng FQ, Xu R, Xia JD, He MR. ECG patterns indicate severity of acute pulmonary embolism: Insights from serial ECG changes in a patient treated with thrombolysis. Visual Diagnosis in Emergency Medicine. 2017; 52: E251-E253.
- Lin JF, Li YC, Yang PY. A case of massive pulmonary embolism with ST elevation in leads V1-V4. Circ J. 2009; 73: 1157-1159. PubMed: https://pubmed.ncbi.nlm.nih.gov/19096187/
- Ghatak A, Alsulaimi A, Acosta YM, Ferreira A. Acute pulmonary embolism masquerading as acute myocardial infarction. Proc (Bayl Univ Med Cent). 2015; 28: 69-70. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4264717/
- Bhatia N, Vongooru H, Ikram S. Acute myocardial infarction and massive pulmonary embolus presenting as cardiac arrest: Initial rhythm as a diagnostic clue. Case Rep Emer Med. 2013; 2013: 343918. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3728547/
- Piggott Z, Jelic T. Pulmonary embolism with cardiac arrest: a STEMI patient’s unexpected course. CJEM. 2018; S31-S36. PubMed: https://pubmed.ncbi.nlm.nih.gov/28875864/
- Vanke P, Nordseth T, Loennechen JP, Mostad DH, Skjaerpe T, et al. A young woman with cardiac arrest. Idsskrift for den Norske Laegeforening.
- Mohsen A, El-Kersh K. Variable ECG findings associated with pulmonary embolism. BMJ Case Rep. 2013; 2013: bcr2013008697. PubMed: https://pubmed.ncbi.nlm.nih.gov/23449833
- Dasa O, Ruzieh M, Ammari Z, Syed MA, Brickman KR, et al. It’s a ST elevation myocardial infarction (STEMI), or is it? Massive Pulmonary Embolism Presenting as STEMI. J Emerg Med. 2018; 55: 125-127. PubMed: https://pubmed.ncbi.nlm.nih.gov/29731284/
- Lu CR, Chen JY, Hsu CH, Chang KC, Huang SKS. Acute massive pulmonary embolism after radiofrequency catheter ablation. Texas Heart Institute J. 37: 498-499. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2929862/
- Hsieh YK, Siao FY, Chiu CC, Yen HH, Chen YL. Massive pulmonary embolism mimicking acute myocardial infarction: Successful use of extracorporeal membrane oxygenation support as bridge to diagnosis. Heart, Lung and Circulation. 2016; 25: e78-e80.
- Hodkinson EC, Noad RL, Menown IBA. Massive pulmonary embolus presenting with abdominal pain. Ulster Med J. 2012; 81: 98. PubMed: https://pubmed.ncbi.nlm.nih.gov/23526855/
- Falterman TJ, Martinez JA, Daberkow D, Weiss LD. Pulmonary embolism with ST segment elevation in leads V1 to V4: Case report and review of the literature regarding electrocardiographic changes in acute pulmonary embolism. J Emerg Med. 2001; 21: 255-261. PubMed: https://pubmed.ncbi.nlm.nih.gov/11604280/
- Yu HH, Jeng JR. Pulseless activity in acute massive pulmonary embolism during thrombolytic therapy. Tzu Chi Med J. 2017; 29: 50-54.
- Idris A, Tong A. Pulmonary embolism mimicking acute AT-segment elevation myocardial infarction. JACC. 2018; 71: 1241-145.
- Bottinor W, Turlinton J, Roberts CS, Malhotra R, Jovin IS, Abbate A. Life-Saving Systemic Thrombolysis in a Patient with Massive Pulmonary Embolism and a Recent Hemorrhagic Cerebrovascular Accident. Tex Heart Inst J. 2014; 41: 174-176. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4004492/
- Valderrey FP, del Ojo JV, Lopez FJA, Millan EM, Cumplido MC, et al. Massive pulmonary embolism and cardiac arrest complicating a stab wound to the heart. Injury Extra. 2011; 42: 171-172.
- Glancy DL. Syncope and dyspnoea and pulmonary embolism. Am J Cardiol. 2016; 118: 463-464.
- Zhong-Qun Z, Chong-Guan W, Nikus KC, Sclarovsky S, Cho-Rong H. A new electrocardiogram finding for massive pulmonary embolism: ST elevation in lead aVR with ST depression in leads and V4-V6. Am J Emerg Med. 2013; 31: 456 -456.
- Willis SL, Welch TS, Scally JP, Bartoszek MW, Sullenberger LE, et al. Impending paradoxical embolism presenting as a pulmonary embolism, transient ischemic attack, and myocardial infarction. CHEST. 2007; 132: 1358-1360. PubMed: https://pubmed.ncbi.nlm.nih.gov/17934122/
- Ramineni R, Daniel G. Association of a patent foramen ovale with myocardial infarction and pulmonary emboli in a peripartum woman. Am J Med Sci. 2010; 340: 326-328. PubMed: https://pubmed.ncbi.nlm.nih.gov/20827172/
- Chen Z, Li C, Li Y, Tang H, Rao L, et al. Concomitant coronary and pulmonary embolism associated with patent foramen ovale. Medicine. 2017; 96: e9480. PubMed: https://pubmed.ncbi.nlm.nih.gov/29384941/
- Smith JG, Koul S, Roijer A, Holmqvist J, Keussen I, et al. Acute right ventricular failure caused by concomitant coronary and pulmonary embolism: successful treatment with endovascular coronary and pulmonary thrombectomy. Eur Heart J Cardiovasc Care. 2013; 2: 131-136. PubMed: https://pubmed.ncbi.nlm.nih.gov/24222822/
- Ferreira AR, Freitas A, Magno P, Soares AO, Abreu PF, et al. Acute coronary syndrome of paradoxical origin. Revista Portuguesa de Cardiologia. 2013; 32: 817-821.
- Hayiroglu M, Bozbeyoglu E, Akyuz S, Yildiyimturk O, Bozbay M, et al. Acute myocardial infarction with concomitant pulmonary embolism as a result of patent foramen ovale. Am J Emerg Med. 2015; 33: 984-984.
- Tukaye DN, Cavallazzi. Paradoxical thromboembolism/ST-elevation myocardial infarction via a patent foramen ovale in submassive pulmonary embolism following an upper extremity deep venous thrombosis: Is it time for a change in the standard of care? Cardiol Res. 2014; 5: 112-117. PubMed: https://pubmed.ncbi.nlm.nih.gov/28348707/
- Alkhalil M, Cahill TJ, Boardaman H, Choudhury RP. Concomitant pulmonary embolism and myocardial infarction due to a paradoxical embolism across a patent foramen ovale: A case report. Eur Heart J Case Rep. 2017; 1: 1-4. PubMed: https://pubmed.ncbi.nlm.nih.gov/31020069/
- Marcu CB, Israel DH, Donohue TJ. Paradoxical coronary embolism, extensive pulmonary embolism and deep venous thrombosis. J Invasive Cardiol. 2005; 17: 487-488.
- Hline A, Malik N, Khokhar A, Affarwal R. Acute myocardial infarction caused by paradoxical embolism with concomitant pulmonary embolism. BMJ Case Rep. 2011; 2011: PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4545089/
- Woo JS, Chung H, Kim WS, Kim W. Embolic myocardial infarction with massive pulmonary thromboembolism. Korean Circulation J. Korean Circ J. 2017; 47: 420–421. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5449539/
- Hakim FA, Kransdorf EP, Abudiab MM, Sweeney JP. Paradoxical coronary artery embolism: A rare cause of myocardial infarction. Heart Views. 2014; 15: 124-126.PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4348985/
- Abecasis, Ribeiras R, Gabriel HM, Andrade MJ. Thrombus entrapment: the clue for coronary embolism. Eur Heart J. 35: 2971. PubMed: https://pubmed.ncbi.nlm.nih.gov/24906617/
- Rivas CG, Sharma A, Arora B, Jaiswal A. Paradoxical coronary embolism in the setting of PFO. JACC. 2020; 75: 3165.
- Cvetkovic D, Zivkovic V, Nokolic S. Patent foramen ovale, paradoxical embolism and fatal coronary obstruction. Forensic Science, Medicine and Pathology.
- Tang L, Fang ZF, Zhou SH. Paradoxical embolism causing acute embolic events in a patient with hereditary thrombophilia. Herz. 2015; 40: 314-317.
- Almehnadi FS, Mehdar AM, Sridhar K, Teefy P. ST-elevation myocardial infarction secondary to paradoxical coronary emboli in a patient with massive pulmonary embolism and essential thrombocytosis: A case report. Int J Case Rep Images. 2015; 6: 149-155.
- Ediban C, Morgan DJ, Rao SV, Keren A, Deague J. Deep vein thrombosis and ftal paradoxical embolism after delyed reduction of a traumatic hip dislocation. J TRAUMA Injury, Infection and Critical Care. 2008; 64: 1133-1135. PubMed: https://pubmed.ncbi.nlm.nih.gov/17413519/
- De Agular DL, Bezerra GN, Plens ICM, de Sousa Belem L, da Costa Lino DO. Thrombus in transit and paradoxical embolism in patient with ST-segment elevation acute coronary syndrome. Arq Bras Cardiol: Imagem cardiovasc 2018; 31: 283-286.
- Onsea K, Bogaard FW, Asselbergs FW, Stella PR. Simultaneous Pulmonary, cerebral and coronary emboli. Int J Cardiol. 2012; 157: e18-e20.
- Stortecky S, Cook S, Meier B. Patent foramen ovale. A culpable pathway for myocardial infarction. JACC. 2011; 58: 1923. PubMed: https://pubmed.ncbi.nlm.nih.gov/22018303/
- Islam AS, Khaligi K, Goldstein JE, Raso J. Paradoxical embolism-Report of a case involving four organ systems. J Emerg Med. 2000; 19: 31-43.
- Falcetta G, Scioti G, Barzaghi C, Bortolotti U. Pulmonary and paradoxical coronary embolism with a patent foramen ovale. Asian Cardiovascu Thoracic Annals. 2018; 26: 413-415.
- Delvigne M, Vermeersch P, van den Heuvel P. Thrombus-in-transit causing paradoxical embolism in cerebral and coronary arterial circulation. Acta Medica Belgica. 2004; 59: 669-672. PubMed: https://pubmed.ncbi.nlm.nih.gov/15636454/
- Mirachi FL, Hecker J, Kramer CM. Pulmonary embolism complicated by patent foramen ovale and paradoxical embolization. J Emerg Med. 2000; 19: 27-30. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3503354/
- Barros-Gomes S, El Sabbagh A, Eleid MF, Mankad SV. Concomitant acute stroke, pulmonary and myocardial infarction due to in-transient thrombus across a patent foramen ovale. Echo Res Practice. 2018; 5: 19-110. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6130432/
- Zhang HY, Zhang Y, Cao YJ., Mei LL, Zhang X, et al. Acute inferior ST elevation myocardial infarction and previous cryptogenic stroke caused by a paradoxical embolism with a concomitant pulmonary embolism. J Geriatric Cardiol. 2017; 14: 421-424.
PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5540877/ - Yee J., Kumar V., Pham A., Shaik K., Omar MStys A, et al. Simultaneous onset of deep vein thrombosis, pulmonary embolism, cerebral infarction and myocardial infarction in a patient with patent foramen ovale South Dakota. J Med. 2017; 70: 266-269. PubMed: https://pubmed.ncbi.nlm.nih.gov/28813763/
- Rovner A, Valika AA, Kovacs A, Kates AM. Possible paradoxical embolism as a rare cause of an acute myocardial infarction. ECHOCARDIOGRAPHY. 2006; 23: 407-409.
- Huang G, Pavan D, Antonini-Canterin F, Piazza R, Cassin M, et al. Thrombus in the right atrial appendage during pulmonary and paradoxical embolism: a case report. Ital Heart J. 2002; 3: 486-489. PubMed: https://pubmed.ncbi.nlm.nih.gov/12407828/
- Lak HM., Ahmed T., Nair R., Maroo A. Simultaneous multifocal embolism in an elderly patient with patent foramen ovale: A case report. CUREUS. 2020; 12: e6992. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7077121/
- Hayman S, Dooris M. Paradoxical coronary embolism and tight to left shunting. Heart Lung and Circulation. 2015: 24: Suppl 3: S387-S388.
- Pilgrim T, Meier B, Khattab AA, Death by patent foramen ovale in a soccer player. J Invasive Cardiol. 2013; 25: 162-164. PubMed: https://pubmed.ncbi.nlm.nih.gov/27047287/
- Nazerian P, Mueller C, Vanni S, de Matos Soeiro A, Leidel BA, et al. Integration of transthoracic focused cardiac ultrasound in the diagnostic algorithm for suspected acute aortic syndromes. Eur Heart J 2019; 40: 1952-1960.
- Dabbousseh NM, Patel J, Bergi PA. Role of echocardiography in managing acute pulmonary embolism. Heart. 2019; 105: 1785-1792. PubMed: https://pubmed.ncbi.nlm.nih.gov/31439657/
- Berg J, Bjorck L, Dudas K, Lappas G, Rosengren A. Symptoms of a first acute myocardial infraction in women and men. Gender Med. 2009; 6: 454-460. PubMed: https://pubmed.ncbi.nlm.nih.gov/19850241/
- Draper J, Subbiah S, Bailey R. Chambers Murmur clinic: validation of a new model for detecting heart valve disease. Heart. 2019; 105: 56-59.
- Hamirani YS, Dietl CA, Voyles W, Peralta M, Begay D, et al. Acute aortic regurgitation. Circulation. 2102; 126: 1121-1126.
- De Martino RR, Sen I, Huang Y, Bower TC, Oderich GS, et al. Population based assessment of the incidence of aortic dissection, intramural hematoma, and penetrating ulcer, and its associated mortality from 1995-2015. Circulation : Cardiovascular Quality and Outcomes. 2018; 11; e004689. PubMed: https://pubmed.ncbi.nlm.nih.gov/30354376
- Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolysis. 2016; 41: 3-14. PubMed: https://pubmed.ncbi.nlm.nih.gov/26780736/
- Neri E, Toscano T, Papalia U, Frati G, Massetti M, et al. Proximal aortic dissection with coronary malperfusion: presentation, management, and outcome. J Thorac Cardiovasc Surg. 2001; 121: 552-560. PubMed: https://pubmed.ncbi.nlm.nih.gov/11241091/
Figures:
Similar Articles
-
Atypical manifestations of pulmonary embolismOscar MP Jolobe*. Atypical manifestations of pulmonary embolism. . 2020 doi: 10.29328/journal.avm.1001012; 4: 008-018
-
Clinical characteristics in STEMI-like aortic dissection versus STEMI-like pulmonary embolismOscar MP Jolobe*. Clinical characteristics in STEMI-like aortic dissection versus STEMI-like pulmonary embolism. . 2020 doi: 10.29328/journal.avm.1001013; 4: 019-030
Recently Viewed
-
Gentian Violet Modulates Cytokines Levels in Mice Spleen toward an Anti-inflammatory ProfileSalam Jbeili, Mohamad Rima, Abdul Rahman Annous, Abdo Ibrahim Berro, Ziad Fajloun, Marc Karam*. Gentian Violet Modulates Cytokines Levels in Mice Spleen toward an Anti-inflammatory Profile. Arch Asthma Allergy Immunol. 2024: doi: 10.29328/journal.aaai.1001034; 8: 001-006
-
A Resurgence of the Idea of Hypertriglyceridemia and Lower Serum (HDL-C) as Predictive Factors for Insulin Resistance (IR) & Type 2 Diabetes Mellitus Development: A Narrative ReviewKulvinder Kochar Kaur*. A Resurgence of the Idea of Hypertriglyceridemia and Lower Serum (HDL-C) as Predictive Factors for Insulin Resistance (IR) & Type 2 Diabetes Mellitus Development: A Narrative Review. New Insights Obes Gene Beyond. 2025: doi: 10.29328/journal.niogb.1001022; 9: 001-012
-
Novel Mutation in Famous Gene Diseases in Red Blood CellsMahdi Nowroozi*. Novel Mutation in Famous Gene Diseases in Red Blood Cells. New Insights Obes Gene Beyond. 2025: doi: 10.29328/journal.niogb.1001023; 9: 013-020
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024: doi: 10.29328/journal.acem.1001030; 8: 004-012
-
The Role of Genetic Mutations in the HPGD & SLCO2A1 Genes in Pachydermoperiostosis SyndromeShahin Asadi*,Arezo Zare,Sima Koohestani. The Role of Genetic Mutations in the HPGD & SLCO2A1 Genes in Pachydermoperiostosis Syndrome. J Genet Med Gene Ther. 2025: doi: 10.29328/journal.jgmgt.1001013; 8: 001-005
Most Viewed
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."